Introduction
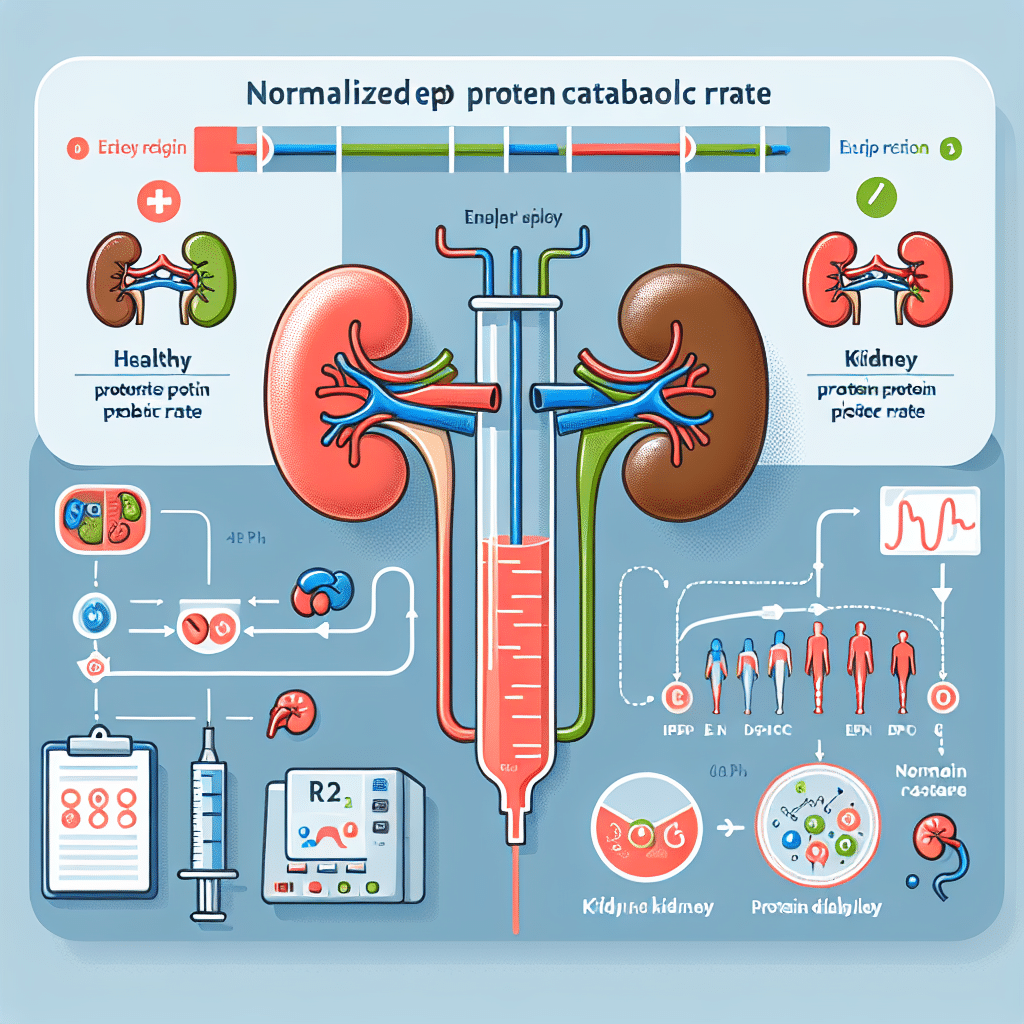
ENPCR, or Effective Nitrogen Production and Clearance Rate, is a pivotal metric in kidney dialysis that assesses the efficacy of treatment related to nitrogen waste removal from the body. In patients with end-stage renal disease (ESRD), the kidneys are unable to filter waste effectively, necessitating dialysis. ENPCR provides healthcare professionals with insights into the patient’s metabolic state and overall kidney function during dialysis sessions. By monitoring this metric, clinicians can tailor treatment plans to improve outcomes, nutrient balance, and overall patient well-being. Understanding ENPCR is essential for both patients and caregivers to ensure proper management of dialysis and better health outcomes.
What is ENPCR?
The Effective Nitrogen Production and Clearance Rate (ENPCR) is a clinical parameter used to evaluate the effectiveness of dialysis in patients with compromised kidney function. This parameter focuses on the clearance of nitrogenous waste products, primarily urea and creatinine, which accumulate in the bloodstream due to inadequate kidney function. ENPCR serves as a vital indicator for adjusting dialysis prescriptions and ensures that patients receive adequate dialysis treatment to maintain metabolic equilibrium.
Understanding Kidney Dialysis
Kidney dialysis is a life-sustaining treatment for individuals diagnosed with end-stage renal disease (ESRD) or severe chronic kidney disease (CKD). The primary purpose of dialysis is to perform the functions that the failing kidneys can no longer manage, notably filtering and removing waste products and excess fluids from the blood. There are two primary types of dialysis: hemodialysis and peritoneal dialysis.
Hemodialysis
During hemodialysis, a machine called a dialyzer filters the blood outside of the body. Blood is drawn from the patient, sent through the dialyzer, and returned after being filtered. This process typically occurs in outpatient centers or at home, depending on the patient’s health status and preference.
Peritoneal Dialysis
Peritoneal dialysis uses the lining of the abdominal cavity (peritoneum) as a natural filter. A special fluid called dialysate is introduced into the abdomen, where it absorbs wastes before being drained away. This method can be performed at home and offers more flexibility to patients.
The Importance of Measuring ENPCR
Measuring ENPCR is crucial for several reasons:
1. Monitoring Dialysis Adequacy
Healthcare providers keep track of ENPCR to ensure that the dialysis treatment is removing enough nitrogenous waste from the patient’s blood. An insufficient ENPCR can lead to the accumulation of toxins, resulting in potential complications.
2. Tailoring Treatment Plans
By evaluating ENPCR levels, healthcare professionals can tailor dialysis protocols, adjust the frequency of treatments, or modify dialysate compositions based on the patient’s individual needs.
3. Optimizing Nutritional Status
Patients undergoing dialysis often struggle with nutritional deficiencies. Monitoring ENPCR can help to identify issues with protein metabolism, guiding adjustments in dietary plans that promote better overall health.
4. Improving Clinical Outcomes
Regular measurement of ENPCR allows for timely interventions to improve patient outcomes, such as reducing hospitalizations and enhancing the quality of life. This proactive approach emphasizes the need for continuous monitoring in ESRD patients.
Factors Influencing ENPCR
Several factors can affect the ENPCR in dialysis patients:
1. Dialysis Modalities
The choice between hemodialysis and peritoneal dialysis influences the ENPCR, with hemodialysis generally showing higher clearance rates due to the nature of the treatment.
2. Dialysis Frequency and Duration
More frequent and longer dialysis sessions can lead to improved waste clearance, thereby enhancing ENPCR.
3. Patient-Specific Variables
Individual factors such as age, comorbid conditions (e.g., diabetes, hypertension), and unique physiological characteristics can significantly impact ENPCR levels.
4. Overall Health Status
Health factors, like inflammation and other diseases, can affect metabolism, thus influencing the effective removal of nitrogenous wastes.
Analyzing ENPCR Results
Clinical teams analyze ENPCR in conjunction with other laboratory results, such as serum urea concentrations and urine output, to assess the overall effectiveness of dialysis treatments. The ENPCR is usually expressed in terms of milliliters per minute per square meter (mL/min/m²) of body surface area, which helps clinicians understand the patient’s nitrogen removal rate relative to their body size.
Limitations of ENPCR
While ENPCR is an essential metric in assessing dialysis efficacy, it does have limitations:
1. Individual Variability
Different patients may have varied baseline levels of nitrogen production, leading to challenges in standardizing ENPCR values across diverse patient populations.
2. Interpretative Challenges
Interpreting ENPCR results requires careful consideration of other clinical information and diagnostic tools to create an accurate picture of a patient’s health status.
Conclusion
Understanding ENPCR’s role in kidney dialysis is paramount for both healthcare providers and patients facing renal failure. By effectively tracking and interpreting this vital parameter, healthcare professionals can improve treatment efficacy, ensuring that patients receive optimal care and support throughout their dialysis journey.
Frequently Asked Questions (FAQ)
What does ENPCR measure?
ENPCR measures the Effective Nitrogen Production and Clearance Rate, which assesses how effectively dialysis removes nitrogenous waste, especially urea and creatinine, from the bloodstream.
How is ENPCR calculated?
ENPCR is calculated using blood tests that measure the levels of nitrogenous wastes before and after dialysis sessions, factoring in the patient’s body surface area for a standardized result.
What is considered a normal ENPCR rate?
A normal ENPCR rate varies between patients but is generally considered to be at least 1.2-1.5 mL/min/m². However, each patient’s ideal level may differ based on their individual health circumstances.
How often should ENPCR be monitored?
Healthcare providers may monitor ENPCR regularly, often monthly or bi-monthly, to evaluate dialysis efficacy and make necessary adjustments to care plans.
What should I do if my ENPCR is low?
If the ENPCR is found to be low, you should discuss the results with your healthcare team. They may recommend adjusting your dialysis schedule, reassessing your nutrition, or reviewing other relevant health factors.