Introduction
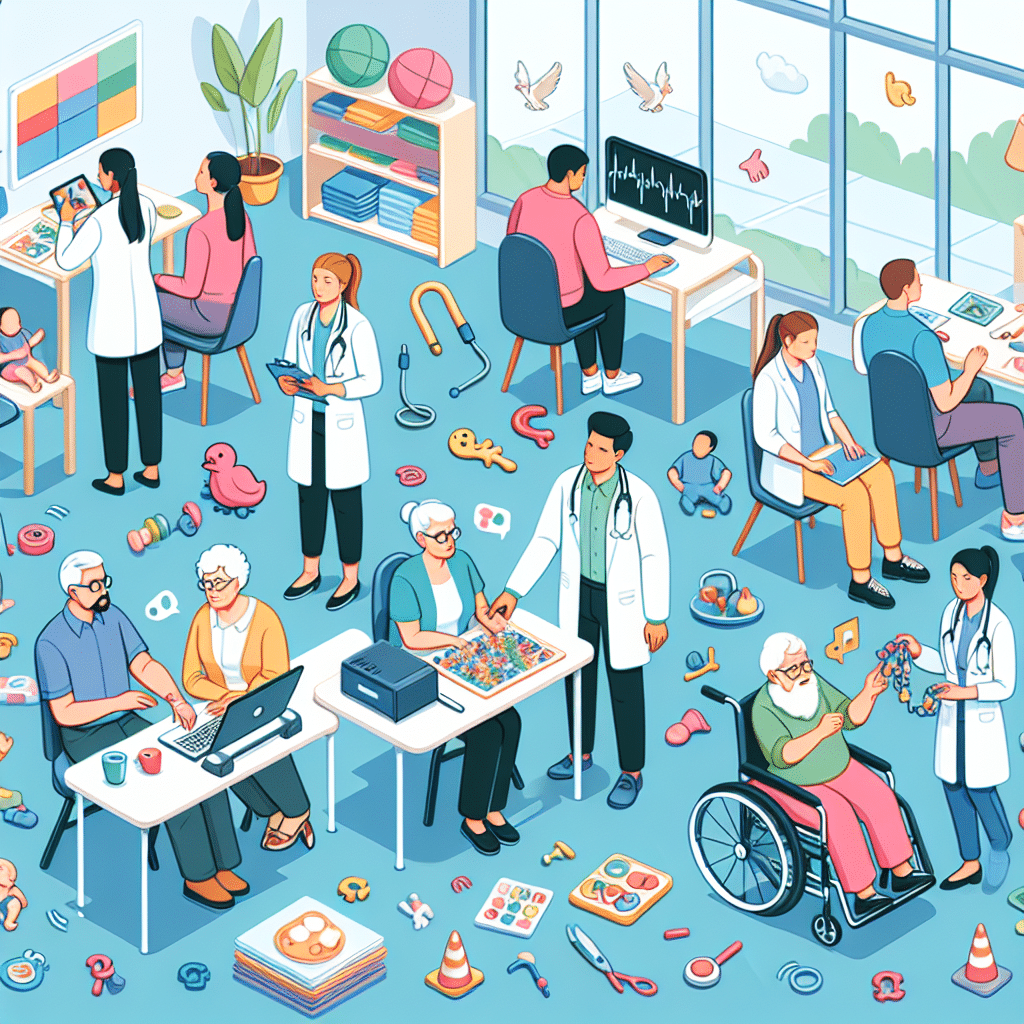
Skilled Nursing Facilities (SNFs) in the realm of speech-language pathology play a crucial role in rehabilitating individuals with communication disorders. These specialized healthcare settings provide comprehensive services tailored to meet the needs of patients recovering from strokes, surgeries, or traumatic injuries affecting their speech and language capabilities. Within an SNF, licensed speech-language pathologists (SLPs) deliver therapeutic interventions designed to enhance communication abilities, improve swallowing function, and promote overall quality of life for residents. By leveraging evidence-based practices, SLPs in SNFs facilitate not only individual recovery but also contribute to the interdisciplinary care that maximizes patient outcomes.
Understanding Skilled Nursing Facilities (SNFs)
Skilled Nursing Facilities, commonly referred to as SNFs, focus on providing high-quality rehabilitation and skilled nursing services to patients who require post-acute care. They cater to individuals with complex medical needs, often following hospitalization, and can include residents with various degrees of physical and cognitive impairments. The objective of an SNF is to support patients in their recovery process, facilitating the transition from hospital to home or to a less intensive level of care.
The Role of Speech-Language Pathologists in SNFs
Within SNFs, speech-language pathologists are vital team members. SLPs assess, diagnose, and treat a wide range of communication and swallowing disorders. They work collaboratively with other healthcare professionals, such as occupational therapists, physical therapists, and nursing staff, to create a tailored care plan for each patient. This integrated approach ensures that all aspects of a patient’s rehabilitation are addressed.
Types of Speech and Language Disorders Treated in SNFs
SLPs in Skilled Nursing Facilities address various disorders, including:
- Aphasia: A language disorder that affects a person’s ability to communicate due to brain damage.
- Dysarthria: A motor speech disorder resulting in unclear articulation due to muscle weakness.
- Dysphagia: Difficulty in swallowing, which can pose risks of choking and aspiration.
Cognitive Rehabilitation in SNFs
Cognitive rehabilitation is another facet of speech-language pathology services in SNFs. Patients may experience cognitive-communication disorders due to neurological conditions such as dementia or post-stroke impairments. SLPs work on enhancing patients’ memory, attention, and problem-solving skills, ultimately supporting their ability to communicate effectively and engage in daily activities.
Rehabilitation Goals and Assessment Process
The rehabilitation process in SNFs typically begins with a comprehensive assessment. This evaluation includes standardized tests and informal observations to gauge a patient’s speech, language, and cognitive abilities. Based on these assessments, SLPs set specific, measurable goals that align with the patient’s needs and desired outcomes. Achieving these goals requires a structured approach, often employing various therapeutic techniques, such as:
- Language exercises: These may include naming tasks, story retelling, and sentence construction.
- Swallowing strategies: Techniques to facilitate safe swallowing, including different posture adjustments and food consistencies.
- Group therapy: Promoting social interaction and communicative competence through structured group activities.
The Importance of Interdisciplinary Collaboration
Successful rehabilitation in SNFs hinges on the collaboration of interdisciplinary teams. SLPs work in harmony with other healthcare providers, sharing insights into patient progress and modifying treatment plans as necessary. This holistic approach ensures that physical, cognitive, and emotional aspects of recovery are considered, creating a comprehensive support system for individuals seeking to regain their independence.
Challenges in SNF Settings
Despite the essential services provided in SNFs, challenges do persist. These may include:
- Staffing shortages: A lack of qualified healthcare professionals can limit the availability of speech therapy services.
- Funding issues: Restrictions in insurance reimbursements can impact the scope of services provided to patients.
- Patient engagement: Some patients may resist therapy due to physical or psychological barriers.
Future of Speech-Language Pathology in SNFs
Looking ahead, advancements in technology and telepractice are poised to enhance speech-language pathology services within SNFs. Remote therapy options can increase accessibility, allowing patients to continue receiving supportive care despite physical limitations. Additionally, ongoing research into best practices and evidence-based interventions will further inform therapeutic approaches, improving outcomes for residents in SNFs.
Frequently Asked Questions (FAQs)
What qualifications do speech-language pathologists have to work in SNFs?
Speech-language pathologists typically hold a master’s degree in speech-language pathology, have completed supervised clinical practice, and possess state licensure and certification from the American Speech-Language-Hearing Association (ASHA).
How can families support loved ones in SNFs?
Families can play a proactive role by engaging in therapy sessions, encouraging communication at home, and participating in care planning meetings. The involvement of family members can significantly impact a patient’s motivation and adherence to therapy.
How do SNFs differ from assisted living facilities?
SNFs provide a higher level of medical care and rehabilitation services, often focusing on patients who have specialized healthcare needs. In contrast, assisted living facilities offer a more independent living environment with minimal medical intervention.